After spiking over the weekend, the number of patients being treated for COVID-19 at Jennie Stuart Medical Center reached a record high of 36 on Monday, hospital spokeswoman Selina Staub confirmed.
The number grew to the previous high of 31 on Saturday — a total reached only once before, on Dec. 23, according to Staub. On Sunday, it increased to 34.

The surge comes as the county’s seven-day average of new cases reached a record high of 56.7 on Saturday, with 397 residents testing positive for the virus over a one-week span.
A previous record-high seven-day average of 47.9 on Dec. 16 and another high of 47.7 a few days later preceded this weekend’s surge in hospitalizations. Health officials have repeatedly pointed out that hospitalizations tend to follow a spike in cases by about two weeks, suggesting the strain on Hopkinsville’s hospital will continue to grow.

During a call with local health officials and members of the media last week, Beth McCraw, Jennie Stuart’s vice president of nursing and clinical services, pointed out that not all patients needing hospital services are reflected in the daily patient totals — those numbers just include coronavirus patients admitted to the hospital. Several others are still seen by the hospital’s emergency department or urgent care.
For the last several months, the strain on the hospital due to the coronavirus pandemic has been unrelenting.
“Our staff is working so hard to care for our community, and they’re tired,” McCraw said Wednesday. “Everybody is tired. We are working to try to identify different ways to help relieve the staff, to get more help … because patients that are sick require a lot more attention than those that are not as sick. We have a lot of folks who are very sick and so it requires a lot of attention from all of our front-line staff. That’s not just our nursing staff, that’s not just clinical staff, that’s everybody provides care in this organization.”
The strain is, in part, because COVID-19 patients require significantly more resources than typical patients. This stems from several factors, including the precautions health care personnel must take before entering coronavirus patients’ rooms, because they are often sicker than typical patients and, frequently, a single nurse is doing tasks that can be difficult for just one person because of the unique challenges posed by patients in isolation.
Updated data released from federal government
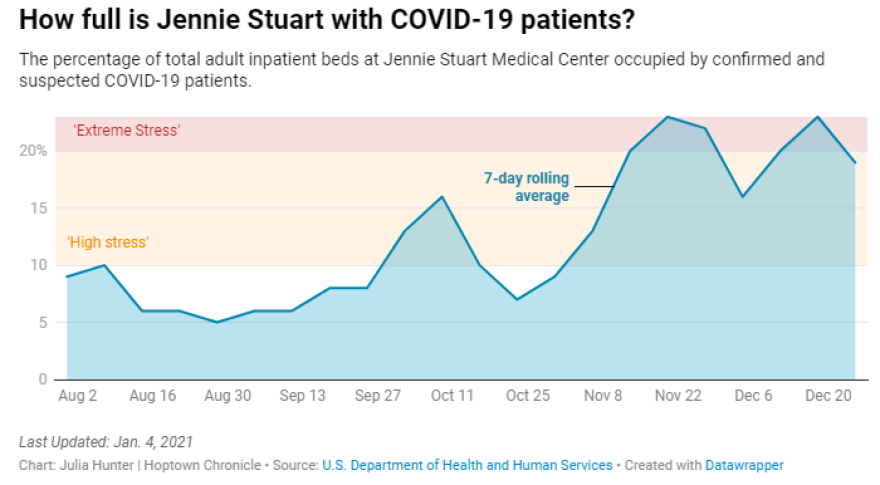
Updated hospital-level data released by the federal government on Sunday show that between Dec. 25 and 31 an average of 19% of adult inpatient beds at Jennie Stuart were occupied by COVID-19 patients. The number is down from the previous week — during which 23% of beds were occupied by patients being treated for coronavirus — but does not include the last three days, when the number of patients being treated for the virus grew to record highs.
According to a framework developed by the Institute for Health Metrics and Evaluation at the University of Washington, 20% is the threshold that indicates a hospital is under “extreme stress.” Anything between 10% and 19% is considered high stress. Jennie Stuart has fallen within the “high” or “extreme” stress threshold since early November.
The data also shows an increase in the total number of patients in the adult intensive care unit. During the week of Dec. 25, the ICU was 67% full on average — a level only exceeded once since August, on Nov. 27, when it reached 69%.
Coronavirus patients comprised, on average, 39% of all patients in the hospital, down from a record high of 50% the week before. They also occupied 40% of ICU beds, up from 29% the week before.
McCraw has noted that non-COVID patients requiring admission to the hospital have been sicker, furthering the strain on local health care workers.
“What we’re seeing is people are sicker now than they have been,” she said Wednesday. “It seems like when people do come in for treatment, they’ve probably postponed it may be a little too long, and whether that’s directly related to the pandemic, I don’t know, but I will say that we are seeing very sick patients.”
(Julia Hunter is the engagement editor for Hoptown Chronicle. Reach her at julia@hoptownchronicle.org.)




