Before Reda Harrison was diagnosed with Alzheimer’s disease, she worked 10-hour days as a surgery coordinator in Lexington.
Always “an organized person,” Harrison “knew something was wrong” when, in 2018, she started feeling confused and lost at work.
Waking at 5 a.m. for work, the Nicholasville woman, 65, said she eventually “made an index card to tell me every step I had to take every morning: brush my teeth, floss…put your makeup on. I had to write it all out, because I would just stand in front of the mirror not knowing what to do.”
Harrison is one of the more than 80,000 Kentuckians aged 65 and older living with an Alzheimer’s diagnosis as reported in the 2025 Alzheimer’s Disease Facts and Figures Report, released by the Alzheimer’s Association last week.
Her husband, Joe, is one of the 160,000 Kentucky residents that the new report says provide unpaid care for a loved one with Alzheimer’s.
Alzheimer’s disease, which falls under the umbrella of dementia, is characterized by memory loss and is incurable, though treatments exist.
One of those treatments underwent clinical trials at the University of Kentucky, Lecanemab (brand name Leqembi). This is an antibody that targets — and in some cases, removes — amyloid plaques from the brain, and has shown some success in slowing cognitive decline. Amyloid plaques are proteins that formin the brain and are believed to be a significant driver of Alzheimer’s. Lecanemab was approved by the U.S. Food and Drug Administration in 2023.
Referring to lecanemab, Mackenzie Wallace, the director of public policy at the Alzheimer’s Association in Kentucky, told the Lantern that this “is an exciting time” for treating the disease.
In March, Senate President Robert Stivers, R-Manchester, announced Kentucky invested $300,000 into space research that will allow the Louisville nonprofit National Stem Cell Foundation to continue researching the way brain cells behave in microgravity in the hopes of finding better treatments — and cures — for Parkinson’s disease, multiple sclerosis and Alzheimer’s.
The money — which was allocated in the 2024 legislative session’s Senate Bill 1 — is a 10% match for a $3.1 million NASA grant.
Scientists hope that research can result in a cure. Meanwhile, this is “the first time in more than 20 years that we actually have a treatment now that is effective at slowing the progression of the disease, and it’s also the first treatment that actually addresses the underlying biology of the disease,” Wallace said of lecanemab.
It’s key to start Lecanemab in the early stages of the disease, making it unsurprising that Tuesday’s report showed most — 79% of Americans surveyed — want to know if they have Alzheimer’s early.
“I think Americans want to know now that it’s becoming less of a taboo or less of a stigma to talk about brain health, and Americans want to know about it, and they want to talk about it,” Wallace said.

By the numbers: what does the new report show?
Shannon White, executive director of the Alzheimer’s Association’s Greater Kentucky and Southern Indiana chapter, called the Tuesday report’s findings “profound.”
“Now more than ever, we need to work to advance disease research and treatments that can slow the current trajectory and help all Kentucky families affected by Alzheimer’s and other dementia,” White said in a statement.
The 2025 Alzheimer’s Disease Facts and Figures Report shows, among other things, a serious need for more geriatricians and more personal aides to care for the 80,500 senior Kentuckians who live with a diagnosis of Alzheimer’s.
There were 48 providers with geriatric certificates in Kentucky in 2021, according to the Facts and Figures report. It estimates Kentucky will need 393 by 2050 to care for all Kentuckians 65 and older and at least 144 geriatricians to care only for those with Alzheimer’s or dementia.
“To meet the increased need and the demand by 2050 we’re going to need a 200% increase in geriatricians,” Wallace said. “And that’s just … almost unfathomable.”
The number of diagnoses are expected to increase as the Baby Boomer generation continues to age. It’s also worth noting, Wallace said, that not everyone who has Alzheimer’s has a diagnosis.
“We know that, still, early detection and diagnosis is a challenge. Even disclosure of diagnosis is still a problem, stigma, denial, etcetera — all of those still impact or affect the ability or desire of people to be able to get a diagnosis. And so the fact that we’re already at 7.2 million people with a diagnosis (nationally) definitely makes you wonder like, wow, how much would that number increase if we kind of thought or were able to measure the people that are at risk, or that have mild cognitive impairment but have not yet been diagnosed?” Wallace said. “I think that’s pretty shocking.”

The report also showed:
- There are 80,500 Kentucky residents aged 65 and older living with Alzheimer’s.
- 10% of adults 65 and older live with Alzheimer’s.
- In 2022, 1,509 Kentuckians died from Alzheimer’s.
- In 2024, there were 160,000 Kentucky residents serving as unpaid family caregivers.
- Those Kentuckians provided 307 million hours of unpaid care worth $4.9 billion.
Among other policies Wallace wants Kentucky to implement, she’d like to see an incentive program for caregivers, similar to the Credit for Caring Act that was introduced in Congress in 2024 that would give eligible caregivers a $5,000 tax credit.
“The cost of this disease is really just staggering,” Wallace said. When it comes to unpaid caregivers, she said, “these are family members, friends, neighbors, loved ones, that are trying to provide care for individuals, for their loved ones.”
If those Kentuckians who are receiving unpaid care were to have to live in nursing homes, Wallace said, “that’s at a great cost to the state” and it’s not as good for the patients.
Meanwhile, Wallace said, unpaid caregivers carry an “all consuming” responsibility.
“If caregivers are out here providing care to their loved one in the home, what does that mean for their own financial well being? Are they dipping into their own retirement funds and savings? Are they having to leave the workforce entirely to provide more care? Are they having to drop down to part time?” Wallace said. “It’s a huge economic toll on caregivers financially, and then on the other side of the coin, it’s a massive toll on our caregivers for their own well being.”
‘You can’t see Alzheimer’s.’
It took Reda Harrison two years to “wrap my arms around” her Alzheimer’s diagnosis. She credits her Christian faith with helping her learn to cope with it and, ultimately, share her story with others.
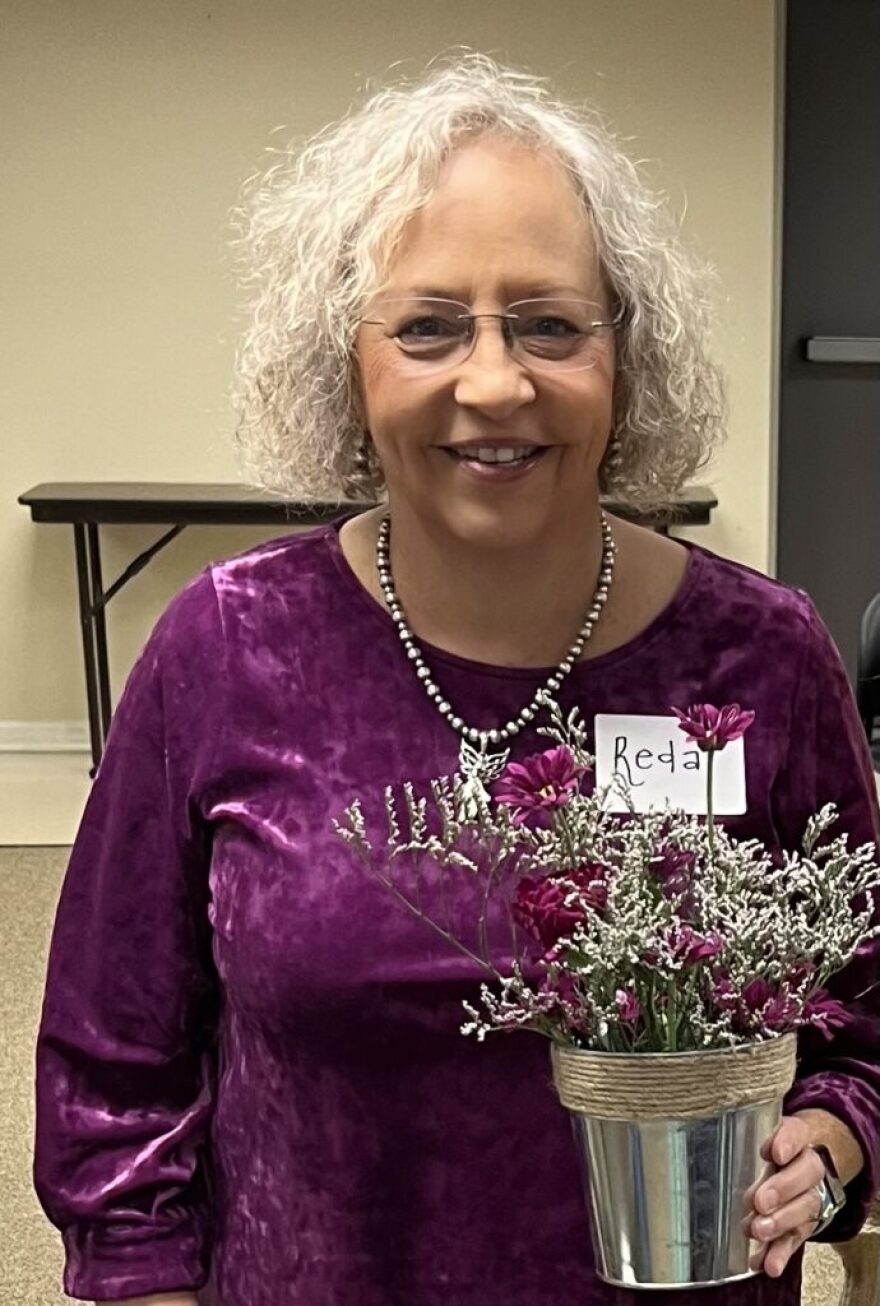
Harrison, who no longer works, attends a support group in Louisville, founded one in Lexington and volunteers with the Alzheimer’s Association.
“Everybody’s case is different. It affects you differently. For me, it was more confusion,” Harrison said. “Since I left work, what I’ve noticed is my short term memory is really bad. I can do something and, a minute later, I can’t remember if I did it or not.”
In addition to attending support groups and volunteering, Harrison fills her time with “anything I can to improve my brain.” She takes piano lessons, studies Spanish on Duolingo, a language learning app, practices yoga, quilts and does beadwork.
Her service dog, Dolly Parton — named after the musician and philanthropist because of the poodle’s “poofy hair” — helps her cope with the depression that comes with her diagnosis. Dolly Parton, the dog, can also help direct her home if she goes for a walk and gets turned around.
“She has really been a lifesaver for me,” Harrison said. “The way she helps me, mostly, is emotional. If I’m having a tough day, she just knows. She’s very comforting, because with this disease, you have a tendency to get depressed. And she helps me.”
Poodle Dolly Parton runs all Harrison’s errands with her as well and loves to be in the car.
“She’s just my companion,” Harrison said. “She keeps me independent.”
Harrison, who is taking Leqembi infusions now, isn’t sure what the future holds for her, or how her Alzheimer’s will progress.

“People decline so differently. Some of the ones that I used to have conversations with can’t even talk anymore. But for me, I really haven’t declined that much. I think it’s just my relationship with God, but I don’t know — there’s no science behind that,” she said. “I’m happy. I have learned to embrace my disease and I don’t run from it. You can’t run from it. You can’t hide from it.”
She wants more people to research Alzheimer’s and educate themselves on it, she said. She believes that’s the key to defeating societal stigma around it.
“People say, ‘Oh, you don’t look like you have Alzheimer’s. You look normal,’” Harrison said. “They don’t know what Alzheimer is. You can’t see Alzheimer’s until you’re far into it.”
Since her diagnosis, she’s lost friends who just felt too uncomfortable with the disease to be around her, she said, saying it felt like “leprosy in the Bible times.” That hurts, and she wants to change negative perceptions of the disease.
“I am still Reda. I am the same person I’ve always been. I’m probably a nicer person now, more caring,” she said. “We still want to be treated for who we are.”
This story was originally published by the Kentucky Lantern.





